Prof. Dr. Niels Olsen Saraiva Câmara
 Academic title: Full Professor
Academic title: Full Professor
Laboratory: Room 238/240
Phone: 55 (11) 3091-7388
E-mail: niels@icb.usp.br
Lattes: http://lattes.cnpq.br/8098379714093877
Researcher ID: http://www.researcherid.com/rid/G-8336-2011
ORCID: https://orcid.org/0000-0001-5436-1248
Site: http://www.icb.usp.br/~niels/
Students / Associated Researchers
Students: Anna Karolina Oliveira (IC), Luís Eduardo Gonçalves (M), Vitor Pedro Targhetta (M), Daniel Marconi (DD), Luisa Menezes Silva (D), Tamisa Seeko Honda (D), Matheus Fragas Garcia (D), Jefferson Antônio Leite (D), Marcella Cipelli (D), Raquel Vieira (D) e Lais Cavalieri (D).
Associated Researchers: Juliana Gomes (PD), Orestes Foresto Neto (PD), Magaiver Andrade (PD), Paulo José Basso (PD), Araceli Hastreiter (PD) e Silviene Novikoff (PD).
Apoio técnico: Meire Ioshie Hiyane (Especialista de Laboratório).
Research Lines
Immunometabolism: Cell metabolism is closely related to phenotypic and functional changes in immune system cells. Glycolysis, lipid beta-oxidation, glutaminolysis and oxidative phosphorylation are used by different cells at different times of differentiation, ontogenesis and polarization. Also, physical modifications in mitochondria, such as fission and fusion, influence the metabolic and functional profile of immune system cells. Similarly, drugs that inhibit or favor one pathway over the other can modify the phenotypic and functional profile of the cells. Control of metabolic pathways is mediated by molecules such as sirtuin and involves epigenetic regulation. Metabolic sensors such as AMPK, mTOR and HIF also modulate this metabolic reprogramming in immune system cell. Finally, metabolic changes can affect fundamental responses to cell survival such as DNA repair pathways. Our group studies these pathways in different inflammation models, including in Zebrafish, with the intention of unraveling the mechanisms involved in crosstalk cellular metabolism-immune response.
Microbiota, obesity, fatty acids and inflammation: In recent years, several national and international research groups, including ours, have consistently shown the role of the inflammatory response in some kidney diseases. Although advances have been more prominent in animal models, the data generated strongly indicate that acute and chronic renal injuries are considered sterile immune response directed against compartments in the nephron. Considered today an epidemic, kidney diseases have high social and economic impact with sustained increased patients’ morbidity and mortality. More recently, new molecules, hormones and cell subtypes have been identified and shown to participate in various inflammatory diseases. With lifestyle changes, new factors have been added to the list of comorbidities for kidney diseases such as obesity. In addition, new hormones related to adipogenicity, changes in intestinal microflora, fermentation products of these bacteria (short chain fatty acids) and inflammatory molecules have all played an important role in the pathophysiology of kidney injury.
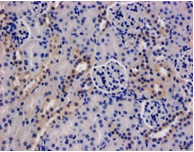
Role of innate and adaptive immune response in acute kidney injury: Ischemia and reperfusion injury (IRI) is the main etiological factor of acute renal injury (AKI), and a strong negative impact factor for the development of chronic nephropathy. Recently, some studies have shown that IRI injury triggers an inflammatory response, involving several cells and molecules of the immune system. We are interested in studying the role of Toll-like, Nod-like and Inflammasome receptors and, specifically, the role of lymphocytes, neutrophils and macrophages in the pathogenesis of this lesion. Our results demonstrate that the TLR4, NOD1 and NLRP3 pathways are early involved in the initial renal injury and that the CD4 + Th1 T lymphocyte subtype is the main aggressor of this lesion.
Zebrafish disease modeling: Zebrafish (Danio rerio), also known as “paulistinha”, has many advantages as an experimental model. Zebrafish has the interesting feature of performing external fertilization with transparent eggs which, when fertilized, develop rapidly and can form a complete embryo within 24 hours. The high regenerative capacity of zebrafish from various organs such as the central nervous system, heart, kidneys and liver, makes the model interesting for studying inflammatory diseases. With respect to the zebrafish immune system, they share mammalian neutrophil-like cells, macrophages, dendritic cells, B and T lymphocytes. The laboratory studies the immune response in inflammatory disease models in Zebrafish as a tool to search for disease mechanisms and actions of new therapeutic drugs.
Stem Cells and Renal Regeneration: Hematopoietic and non-hematopoietic stem cells, mesenchymal stem cells, are cells with sufficient plasticity to regenerate tissues and restore physiological functions in damaged organs. The laboratory studies the immunological mechanisms involved in the movement of these cells into the kidney in models of acute and chronic kidney diseases, their plasticity in differentiating into tubular cells, and their ability to modulate inflammatory response in organ transplant and acute kidney injury models.
Regulatory Cells and Organ Transplantation: Induction of tolerance remains the only strategy to increase graft survival without causing toxic graft damage. CD4 + CD25 + T cells, or regulatory T, and NKT cells have been well characterized in the last decades and have been described in humans, autoimmune diseases, viral infections, tumors and organ transplantation. The laboratory is interested in studying its frequency, its pattern of cytokine production, its specificity and its traffic in humans, especially in kidney transplantation.
Protective genes: heme oxygenase 1 and kidney: Heme oxygenase 1 (HO-1) is considered a protective gene with anti-apoptotic, anti-proliferative and anti-inflammatory activities. Overexpression of HO-1 in kidney undergoing IR limits the damage caused by ischemia. In experimental models of chronic rejection, HO-1 is capable of suppressing atherosclerotic lesions, pathognomonic of chronic injury. However, HO-1 expression may be regulated by a polymorphism in its promoter and by the use of immunosuppressants. The laboratory is interested in studying the role of HO-1 in acute renal injury, and in various clinical situations following renal transplantation, in in vitro models of epithelia-to-mesenchymal transdifferentiation and in vivo acute kidney injury.
Financial Support: FAPESP, CAPES, CNPq, ROTRF, Genzyme, NIH.
Main publications in the last 5 years (http://www.researcherid.com/rid/G-8336-2011)
- Basso PJ, Andrade-Oliveira V, Câmara NOS. Targeting immune cell metabolism in kidney diseases. Nat Rev Nephrol. 2021 Apr 7. doi: 10.1038/s41581-021-00413-7.
- Braga TT, Davanso MR, Mendes D, de Souza TA, de Brito AF, Cruz MC, Hiyane MI, de Lima DS, Nunes V, de Fátima Giarola J, Souto DEP, Próchnicki T, Lauterbach M, Biscaia SMP, de Freitas RA, Curi R, Pontillo A, Latz E, Camara NOS. Sensing soluble uric acid by Naip1-Nlrp3 platform. Cell Death Dis. 2021 Feb 5;12(2):158. doi: 10.1038/s41419-021-03445-w.
- Fachi JL, Sécca C, Rodrigues PB, Mato FCP, Di Luccia B, Felipe JS, Pral LP, Rungue M, Rocha VM, Sato FT, Sampaio U, Clerici MTPS, Rodrigues HG, Câmara NOS, Consonni SR, Vieira AT, Oliveira SC, Mackay CR, Layden BT, Bortoluci KR, Colonna M, Vinolo MAR. Acetate coordinates neutrophil and ILC3 responses against C. difficile through FFAR2. J Exp Med. 2020 Mar 2;217(3). pii: e20190489. doi: 10.1084/jem.20190489.
- Almeida RR, Vieira RS, Castoldi A, Terra FF, Melo ACL, Canesso MCC, Lemos L, Cipelli M, Rana N, Hiyane MI, Pearce EL, Martins FDS, Faria AMC, Câmara NOS. Host dysbiosis negatively impacts IL-9-producing T-cell differentiation and antitumour immunity. Br J Cancer. 2020 Aug;123(4):534-541. doi: 10.1038/s41416-020-0915-6. Epub 2020 Jun 5.
- Wu CJ, Cho S, Huang HY, Lu CH, Russ J, Cruz LO, da Cunha FF, Chen MC, Lin LL, Warner LM, Liao HK, Utzschneider DT, Quon S, Berner J, Camara NOS, Zehn D, Belmonte JCI, Chen LC, Huang SF, Kuo ML, Lu LF. MiR-23~27~24-mediated control of humoral immunity reveals a TOX-driven regulatory circuit in follicular helper T cell differentiation. Sci Adv. 2019 Dec 11;5(12):eaaw1715. doi: 10.1126/sciadv.aaw1715. eCollection 2019 Dec.
- Breda CNS, Davanzo GG, Basso PJ, Saraiva Câmara NO, Moraes-Vieira PMM. Mitochondria as central hub of the immune system. Redox Biol. 2019 Jun 15;26:101255. doi: 10.1016/j.redox.2019.101255. [Epub ahead of print] Review.
- Fachi JL, Felipe JS, Pral LP, da Silva BK, Corrêa RO, de Andrade MCP, da Fonseca DM, Basso PJ, Câmara NOS, de Sales E Souza ÉL, Dos Santos Martins F, Guima SES, Thomas AM, Setubal JC, Magalhães YT, Forti FL, Candreva T, Rodrigues HG, de Jesus MB, Consonni SR, Farias ADS, Varga-Weisz P, Vinolo MAR. Butyrate Protects Mice from Clostridium difficile-Induced Colitis through an HIF-1-Dependent Mechanism. Cell Rep. 2019 Apr 16;27(3):750-761.e7. doi: 10.1016/j.celrep.2019.03.054.
- Correa-Costa M, Gallo D, Csizmadia E, Gomperts E, Lieberum JL, Hauser CJ, Ji X, Wang B, Câmara NOS, Robson SC, Otterbein LE. Carbon monoxide protects the kidney through the central circadian clock and CD39. Proc Natl Acad Sci U S A. 2018 Mar 6;115(10):E2302-E2310. doi: 10.1073/pnas.1716747115. Epub 2018 Feb 20.
- Angela Castoldi; Vinicius Andrade-Oliveira; Cristhiane Favero Aguiar; Mariane Tami Amano; Jennifer Lee; Marcelli Terumi Miyagi; Marcela Teatin Latância; Tarcio Teodoro Braga; Marina Burgos Da Silva; Aline Ignácio; Joanna Darck Carola C. Lima; Flavio V. Loures, José Antonio T. Albuquerque; Marina Barguil Macêdo; Rafael Ribeiro Almeida; Jonas W. Gaiarsa; Luis A. Luévano Martínez; Thiago Belchior; Meire Ioshie Hiyane; Gordon D. Brown; Marcelo A. Mori; Christian Hoffmann; Marília Seelaender; Willian T. Festuccia; Pedro Manoel Moraes-Vieira; Niels Olsen Saraiva Câmara. Dectin-1 activation exacerbates obesity and insulin resistance in absence of MyD88. Cell Rep. 2017 Jun 13;19(11):2272-2288. doi: 10.1016/j.celrep.2017.05.059.
- Câmara No, Iseki K, Kramer H, Liu Zh, Sharma K. Kidney disease and obesity: epidemiology, mechanisms and treatment. Nat Rev Nephrol. 2017 Mar;13(3):181-190. doi: 10.1038/nrneph.2016.191.Breda CNS, Davanzo GG, Basso PJ, Saraiva Câmara NO, Moraes-Vieira PMM. Mitochondria as central hub of the immune system. Redox Biol. 2019 Jun 15;26:101255. doi: 10.1016/j.redox.2019.101255. [Epub ahead of print] Review.
Copyright © 2025 Programa de Pós-Graduação em Imunologia | Produzido por SCS - Mídias Online